How I Feed My Chickens and Why Pasture-Raised is Not Good Enough
The Urgent Issue: Excess Linoleic Acid and Excess OxLAMs
One of the problems of the modern lifestyle that has helped to destroy our health is the excess linoleic acid in our diets. Linoleic acid (18:2 N6 and is not to be confused with linolenic acid or alpha-linolenic acid) is an essential omega-6 polyunsaturated fatty acid that plays a crucial role in our bodies’ structure, particularly in the formation of cell membranes, and as a signaling molecule, involved in various physiological processes. Quoting an article in Nature by Ameer Y. Taha:
Linoleic acid (LA, 18:2n-6) is an essential n-6 polyunsaturated fatty acid (PUFA) required for normal growth and development at 1 to 2% of daily energy. LA has become ubiquitous in Western diets over the past few decades due to agricultural shifts towards high-LA soybean and corn oils during the late 1930s, resulting in a greater than 3-fold increase in intake. Historic levels of LA intake ranged between 1 to 2% of daily calories pre-1930s, but currently average more than 7% of daily calories. Based on economic disappearance data, the majority of LA in the US diet comes from soybean oil.
Amongst other dietary PUFAs important for optimal health, LA is the only one that has markedly changed in the diet over the past few decades. Contrary to common misconception, the intake of LA’s elongation-desaturation product, arachidonic acid (AA, 20:4n-6), and the essential n-3 fatty acid, alpha-linolenic acid (ALA, 18:3n-3), and its elongation-desaturation products eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), has remained relatively constant at <1% energy since the early 1900s. Excess LA in the food supply has shifted the n-6 to n-3 ratio from 4:1 to 20:1.
The author goes on in the paper to describe some of the associations found with linoleic acid:
Ramsden et al. reported that dietary LA lowering from 7% to 2% energy combined with a high EPA and DHA diet (~1.5 g per day) for 12 weeks, reduced migraine frequency and improved quality of life in patients with drug-resistant migraines. Lowering dietary LA without changing EPA and DHA did not significantly alter migraine frequency or improve quality of life. Although this study did not have a parallel group that received EPA and DHA alone, it provides evidence of a potential synergistic benefit to lowering LA and increasing EPA and DHA simultaneously. It is possible that longer-term LA lowering regimens might reduce migraine frequency as well, although this remains to be tested.
Several epidemiological studies explored the role of LA on neurodevelopment. Like other dietary fatty acids, LA accumulates in breast milk, which is the primary source of infant nutrition for the first few months of life. Thus, consistent with the increase in dietary LA in the food supply, breastmilk LA composition has increased from 7% to 12% of total fatty acids between 1970 and 2000. The 12% composition value corresponds to 8% energy, which exceeds the minimum 1–2% energy required for developing infants by 4–8-fold.
Overall, studies have shown an adverse effect of maternal breast milk or dietary LA on neurodevelopment. One study reported that a high maternal breast milk LA percent composition (>9.7% of fatty acids) was associated with reduced motor and cognitive scores in 2- to 3-year-old infants. In the same cohort, maternal breastmilk LA percent composition was associated with reduced verbal IQ at 5 to 6 years of age. In fact, children breastfed with the highest levels of LA had cognitive scores comparable to children who were never breastfed. These effects were independent of AA or DHA breast milk composition, suggesting a direct impact of excess breast milk LA (and hence maternal intake) on brain development. Consistent with these findings, Lassek and Gaulin found an inverse correlation between breast milk LA percent composition and cognitive scores in 15-year-old children, suggesting a long-lasting impact of maternal LA on offspring cognitive skills. Steenweg-de Graaff et al. also reported a significant positive association between maternal plasma LA composition measured at mid-pregnancy and the risk of autistic traits in children at the age of 6 years. A more recent study found that prenatal intake of diets high in the ratio of LA to ALA, was associated with a 2-fold increase in the risk of delayed psychomotor and mental developmental in 6 months infants.
However, the problem with excess linoleic acid comes from excess oxidized linoleic acid metabolites (OxLAMs). Inflammation is an essential part of how our body functions. It serves as a signal to marshal the proper resources to eliminate injurious stimuli (likely infections) and to heal injury. For fans of The Lord of the Rings movies, imagine lighting the beacons of Minas Tirith under normal conditions. You will have a signal allowing Gondor to call for aid, which Rohan will answer. Imagine now that you have an excessive amount of extremely dry wood, with excessive oil to burn, and highly combustible land surrounding the pillar. You get an uncontrolled raging inferno instead of a controlled fire. With so many people suffering from inflammation and its consequences, the chief culprit may be the change in diet over the last century. If the culprit is excess linoleic acid, it should manifest as consequences related to OxLAMs and the development of drugs that work to mitigate those consequences. I’ve included a few examples below.
Linoleic acid undergoes a transformation into one of its OxLAMs, arachidonic acid (AA). This AA is then converted into prostaglandin G2 (PGG2) by the pivotal enzymes COX 1 and 2. Following this, PGG2 is converted to prostaglandin PGH2 (PGH2), from which it can be transformed into various signaling molecules. Image from NSAIDs and Cancer Resolution: New Paradigms beyond Cyclooxygenase
-
As stated by Bergqvist et al., "PGE2 is implicated in all processes leading to the cardinal signs of inflammation, including heat, redness, swelling, and pain, and is an immune modulator via actions on lymphoid and myeloid cells. NSAIDs, including NS-398 and naproxen, are frequently used to treat pain and inflammation due to their COX-specific reduction in prostaglandin biosynthesis...Using NSAIDs to relieve pain in tendinopathy is controversial as these treatments are associated with impaired tendon healing and adverse effects on tendon mechanical properties. Therefore, inhibiting the downstream enzyme in the PGE2 biosynthesis is a potential strategy to selectively target inflammation without the deleterious side effects associated with COX inhibition."
In this case, it appears that NSAIDs are being used to treat the consequences of OxLAMs, specifically the products created from arachidonic acid (AA).
-
Warner et al. write, "Aspirin and P2Y12 antagonists are commonly used anti-platelet agents. Aspirin produces its effects through inhibition of thromboxane A2 (TXA2) production, while P2Y12 antagonists attenuate the secondary responses to ADP released by activated platelets. The anti-platelet effects of aspirin and a P2Y12 antagonist are often considered to be separately additive. However, there is evidence of an overlap in effects, in that a high level of P2Y12 receptor inhibition can blunt TXA2 receptor signalling in platelets and reduce platelet production of TXA2."
An example of a P2Y12 inhibitor is Plavix (clopidogrel). As you can see in the image, TXA2 is derived from PGH2. So those who are using medications like Plavix and aspirin to prevent heart attacks and strokes, they may be using those drugs to treat the consequences of OxLAMS
-
As described in the StatPearls article "Leukotriene Receptor Antagonists,": "The main indication for leukotriene receptor antagonists is in treating chronic asthma. Leukotrienes are synthesized from arachidonic acid by the action of 5-lipoxygenase in many inflammatory cells in the airways...Corticosteroids inhibit phospholipase A2 and subsequent synthesis of eicosanoid inflammatory mediators, including both prostaglandins and leukotrienes...Zileuton inhibits 5-Lipoxygenase...Cysteinyl leukotrienes (LTC4, LTD4, and LTE4) have amino acid moiety and bind to cysteinyl leukotriene receptors (CysLT1 and CysLT2). Bronchoconstriction, vascular permeability, eosinophil recruitment, and chronic inflammation are mediated through the G protein-coupled activation of cysteinyl leukotriene receptors. Montelukast and zafirlukast are antagonists to cysteinyl leukotriene CysLT1 receptors..."
Medications like corticosteroids (prednisone), inhaled corticosteroids (budesonide), Zileuton (Zyflo). Montelukast (Singulair) all work by limiting the production of compounds that are derived from an OxLAM
-
Domingo et al., "Prostaglandin D2 (PGD2) is a lipid mediator, predominantly released from mast cells, but also by other immune cells such as TH2 cells and dendritic cells, which plays a significant role in the pathophysiology of asthma...increased PGD2 production induces significant inflammatory cell chemotaxis and degranulation via its interaction with the DP2 receptor. This interaction has serious consequences in the pulmonary milieu, including the release of pro-inflammatory cytokines and harmful cationic proteases, leading to tissue remodeling, mucus production, structural damage, and compromised lung function."
While there are multiple theorized causes for the rise in asthma over the last 100 years, it may be that diet, particularly excess linoleic acid -> excess arachidonic acid -> excess PGD2 -> asthma.
For More…
I will direct the reader to two articles by Tucker Goodrich on the topic. The first is Omega-6 Fats: The Alternative Hypothesis for Chronic Disease (a Google Drive PDF file). The second is Linoleic Acid and Its Metabolites, a Primer (which is much more technical with respect to the material presented).
Sources of Excess Linoleic Acid
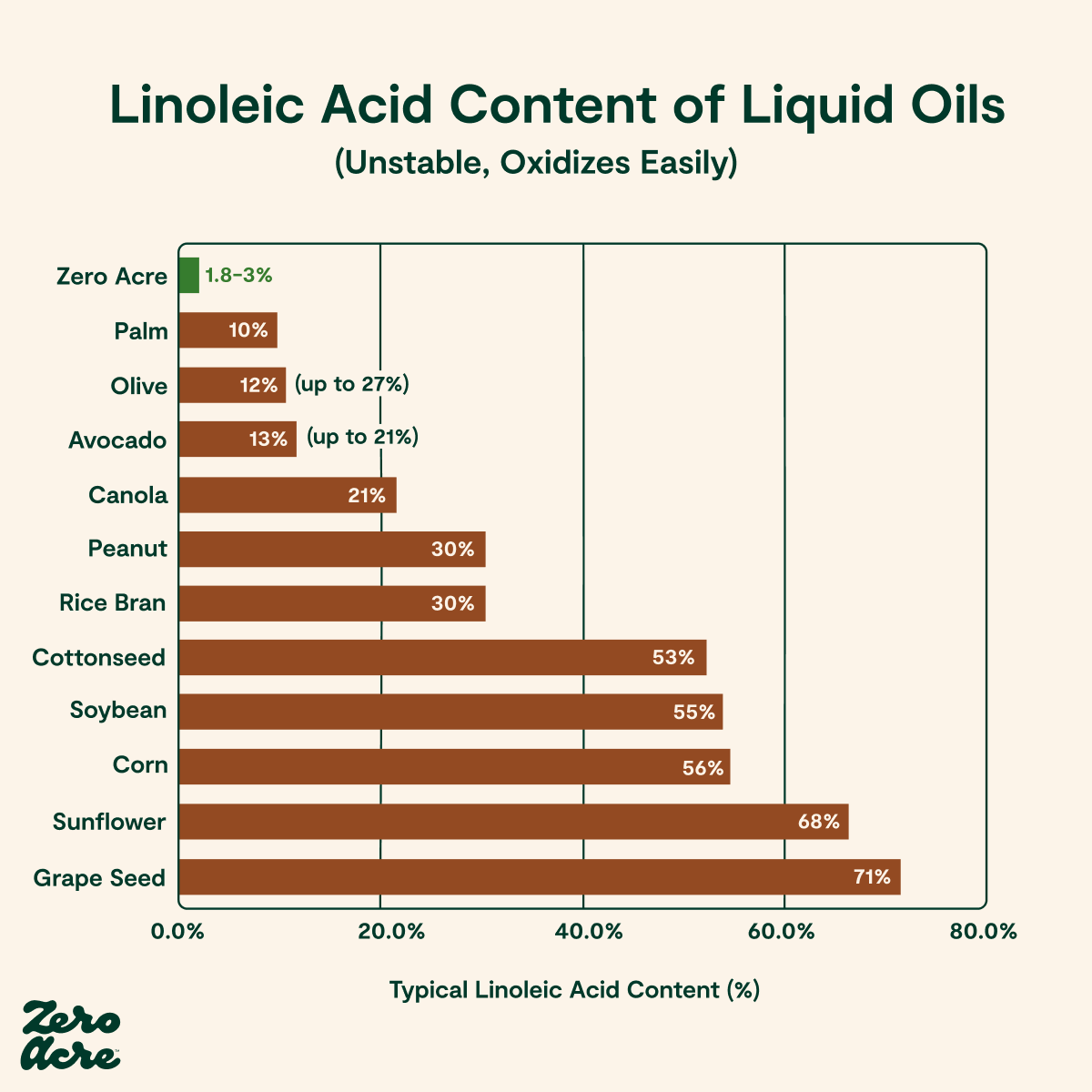
Pound for pound (more gram for gram), seed oils contain the most linoleic acid. Consider what this chart from the Zero Acre blog shows (I have not used their product, nor am I associated with the company or the blog in any way) and that ancestral diets overall were around 2%. We can see how these industrial lubricants-turned-food will wreak havoc on the body in the long run.
Ruminant Animal Fat
Ruminant animals possess a unique digestive system that efficiently breaks down complex plant materials. Their four-chambered stomach comprises the rumen, reticulum, omasum, and abomasum. The primary function of the rumen is to ferment ingested food, which allows ruminants to extract nutrients from fibrous plant matter, such as grasses and leaves. During the fermentation process, ruminants engage in a behavior known as rumination, where they regurgitate and re-chew their food to further break it down before swallowing it again. Common examples of ruminants include cows, sheep, goats, deer, bison, and elk.
A 100% grass-fed ruminant generally has a linoleic acid content of around 2-3% in their fat. This includes butter and fats derived from butter (smen, clarified butter, and ghee). A completely grain-fed ruminant of the same species will often have a similar or slightly higher linoleic acid content, but usually no higher than 4-6%. This is likely a byproduct of rumination. As Dinh et al. write, “Ruminant fatty acid composition is greatly influenced by biohydrogenation in the rumen, which saturates linoleic and linolenic acids, as a protective mechanism from natural microflora against the toxic effects of unsaturated fatty acids.”
Otherwise, though, there are substantial differences in the nutritional value of ruminant meat that is 100% grass-fed vs. the equivalent grain-fed version. For instance, the omega-3/omega-6 ratio, which we will not discuss at this time, is a key indicator of the health benefits of grass-fed meat. Grass-fed meat typically has a more favorable ratio, which is beneficial for human health.
Non-Ruminant Animal Fat
Non-ruminant animals do not have a complex stomach structure for digesting fibrous plant material. Unlike ruminants, such as cows and sheep, which have a multi-chambered stomach, non-ruminants typically possess a single-chamber stomach. Examples are fowl, including chickens, pigs, and horses.
In “Fatty Acid Composition of Meat Animals as Flavor Precursor ", this table shows the marked difference between ruminants and non-ruminant animals concerning linoleic acid (18:2).
Lowering Linoleic Acid in Non-Ruminant Animal Foods
How can we reduce the linoleic acid content of the chicken, eggs, pork, etc. that we eat? Some may argue that we should eat pasture-raised pigs and chickens. However, as shown in Sergin et al.’s work comparing pasture raised eggs fed either 1) beef liver, beef suet, peas, alfalfa, barley, and calcium (PBB), 2) standard corn and soy feed (PCS), with a third group, cage-free eggs that were purchased (CFC) as a comparison, the amount of linoleic acid (18:2 n-6) in the eggs of chickens pasture-raised with corn and soy feed was still an average of 16.19%.
However, the PBB eggs from chickens fed beef liver, beef suet, peas, alfalfa, barley, and calcium had a 7% linoleic acid (18:2 n-6) on average. One can see that even supplementation with 30-60 g of liver per week per hen and ad libitum suet helped to reduce the linoleic acid in the eggs, likely due to a reduction in linoleic acid intake. The liver had fat that was 4.11% linoleic acid. The suet’s linoleic acid concentration was 0.8%. The rest of the PBB feed regimen had a linoleic acid concentration of 51.1% (the corn and soy feed had a concentration of 56.1%).
Enser et al. noted a similar finding in 2000. In this pig-feeding study, they decreased the linoleic acid proportion of fat in the diet from 35.6% to 22.2% while also increasing the alpha-linolenic acid (3.3% to 10.0%) and the palmitic acid (11.1% to 22.2%). The resulting meat had a statistically significant drop in the linoleic acid concentration from 17.5% in female pigs and 17.3% in male pigs to 14.1% in both males and females.
And while black soldier larvae are not on the menu for humans, they are commonly fed to chickens. As Li et al. show that linoleic acid (C18:2 n-6) varies considerably depending on what they are fed, where the higher the linoleic acid in the diet, the higher the linoeic acid in the larvae.
Therefore, while pasture-raising has the potential to improve various nutritious elements of foods, any benefits concerning the linoleic acid levels in non-ruminant animal fats, be it in meat or eggs, are lost if they are fed a high linoleic acid diet.
The Pasture-Raised Egg Landscape
Pasture-raised eggs are becoming a more common fixture in grocery stores. These birds have above 108 square feet per chicken to forage. However, the term “pasture-raised” does not provide any insight into what their supplemental feed contains.
The designation “no-corn, no-soy” does not clearly answer whether the chickens are fed a low PUFA diet. This is because farms often use other seed oils or seed oil meals even if they are no-corn and no-soy. Here are examples of fat sources in feeds available to consumers labeled “no-corn, no-soy”:
Modesto Milling: Sesame meal
New Country Organics: fish meal, flaxseed meal, sunflower oil
Reedy Fork Farm: Flaxseed meal, organic sunflower oil, organic flax oil
Small Pet Select: Sunflower seeds, flax seeds, pumpkin seeds
Garden Betty (a blog, not a commercial feed): black oil sunflower seeds, sesame seeds
H&H Feed: flax seeds, sunflower seeds
Happy Hens, which scored 5/5 eggs by the Cornucopia Institute, sells no-soy, no-corn eggs. They feed their chickens sesame.
How I Feed My Chickens
Many people in the Jacksonville area have chickens. However, part of the reason I bought the home I did was to try to raise low-PUFA pasture-raised eggs.
I need to feed my chicken a low-linoleic acid diet in order to get low-linoleic acid chicken eggs. Their diet consists of grass-fed, grass-finished liver, which I get at $0.60/lb, organic buckwheat groats at $1.36/lb including shipping from Azure, organic field peas at $0.88/lb including shipping from Azure, organic barley at $0.65/lb including shipping from Azure, and organic medium shredded coconut at $1.68/lb including shipping.
With the beef and the coconut, we have low linoleic acid levels, around 2-4% for the liver and around 1-2% for the coconut. Field peas, hulled barley, and buckwheat do not come close to those low levels of linoleic acid. Field peas contain about 35% linoleic acid. Barley contains approximately 57% linoleic acid. Buckwheat groats contain approximately 38% linoleic acid.
Currently, I am experimenting with removing the field peas and substituting them completely with liver. This is to see how the chickens do with the higher-quality protein source during their first molt. Calculating the percentage of linoleic acid in their current feed, it comes to 5.36%.
Currently, I do not have any way of testing the linoleic acid content of the eggs, so I will have to be happy with what I have based on the feed mix I give them.
Food For Thought
There is far more evidence of the problems of excess linoleic acid and of excess oxidized linoleic acid metabolites that I will not cover today. Given this concerning evidence, one step in reversing the consequences of modernity on our health would be to lower our consumption of linoleic acid back to levels consistent with ancestral diets, around 2%. That starts with removing all industrial lubricants (seed oils) from our diets. However, more may be needed due to the high PUFA diets fed non-ruminant animals and the consumption of pork and chicken in the country relative to ruminant meat. To reclaim our health, some of us may have to go so far as to find create an increased supply of low PUFA eggs, chicken, pork, duck, and turkey, or shift back to consuming more ruminant animals at the expense of consuming non-ruminant animals.
If you are interested in improving your health, sign up with Florida Low Carb Direct Primary Care below